HKU Research Team Designs nanoscale Matrix on Titanium Alloy Surface
HKU Research Team Designs Nanoscale Matrix on Titanium Alloy Surface
Recently, the team of the Department of Orthopedic and Trauma Surgery of the Li Ka Shing School of Medicine of the University of Hong Kong, designed a unique honeycomb-like nanoscale matrix on the surface of medical titanium alloy, which can more effectively promote the fusion of titanium alloy implants with bones in the body. The healing time after surgery can be shortened from six to eight months to about two to four months. This discovery can be applied to prosthetics, artificial joints and denture transplantation and other fields.
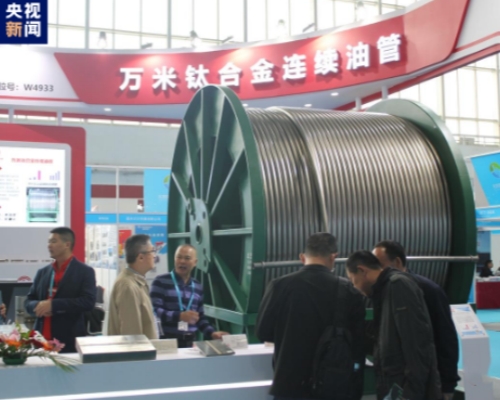
Patients who need amputation usually need to assemble prosthetics through surgery, the main material of most of the instruments is titanium alloy. One of the goals of the surgery is to achieve superior bone and implant fusion as soon as possible, but this fusion will take about six to eight months. According to medical literature, the immune response of the host bone and the implant material is very intense a few hours after the surgery is completed. These unavoidable immune responses will form an immune tissue microenvironment on the connected implant material, thereby manipulating the effectiveness of bone and implant fusion.
The research team designed a series of honeycomb matrix structures from nanoscale to micron on the surface of the titanium alloy, allowing immune cells to grow in the surface space of the material, so as to observe its immune-oriented differentiation. The study found that because the honeycomb structure restricts the growth space of immune cells and affects the skeleton structure within the cells, M0 macrophages (an inactive macrophage immune cell) will differentiate into different cell subtypes in order to adapt to these surface matrices.
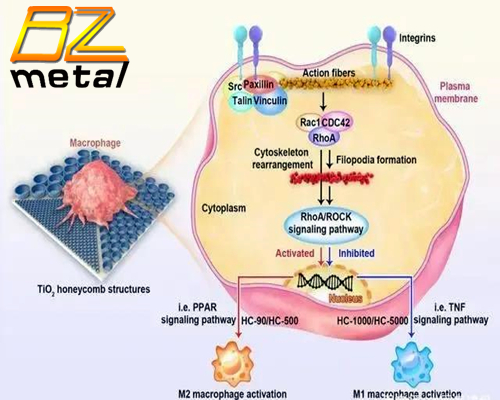
The team found that the 90 nm matrix design can regulate the differentiation of M0 macrophages towards M2 macrophages (an anti-inflammatory macrophage subtype) through the Rhoa/ROCK signaling pathway. In simple terms, the nano-matrix with a size of 90 nm provides minimal space for macrophage growth, which can strengthen the adhesion ability of macrophages on the surface of the material, so that the guanosine triphosphatase (RhoA, Rac1 and CDC42) genes of the Rho family are upregulated, activate the RhoA/ROCK signaling pathway, and regulate the polarization of M0 macrophages to M2 subtypes. This tailor-made immune tissue microenvironment is conducive to the development of mesenchymal stem cells in the direction of osteoblasts, so as to achieve excellent bone and implant fusion.
Professor Yang Weiguo, Department of Orthopedic and Trauma Surgery, Hong Kong University School of Medicine, said: “These nanostructures can be applied to prosthetics, artificial joints and even denture transplants, reducing the fusion time between bones and implants by up to two-thirds. In total joint replacement surgery, these structures are also suitable for cobalt-chromium alloy and other implant materials. Depending on the results of further research and clinical trials, these honeycomb structures may be used to carry drugs such as analgesics and antibiotics in the future. ”